“To better assess the state of primary care in the U.S., [The Physicians Foundation] worked with the Milbank Memorial Fund to release the first-ever national primary care scorecard in February of 2023. This initial scorecard provided a benchmark of the state of primary care and found that underinvestment, workforce shortages and lack of research funding threaten this essential sector of health care. The scorecard also included necessary recommendations to address the challenges faced by primary care physicians, pointing the way towards a future in which primary care is better supported and all patients can live healthier lives.” (The Physicians Foundation, 2024)
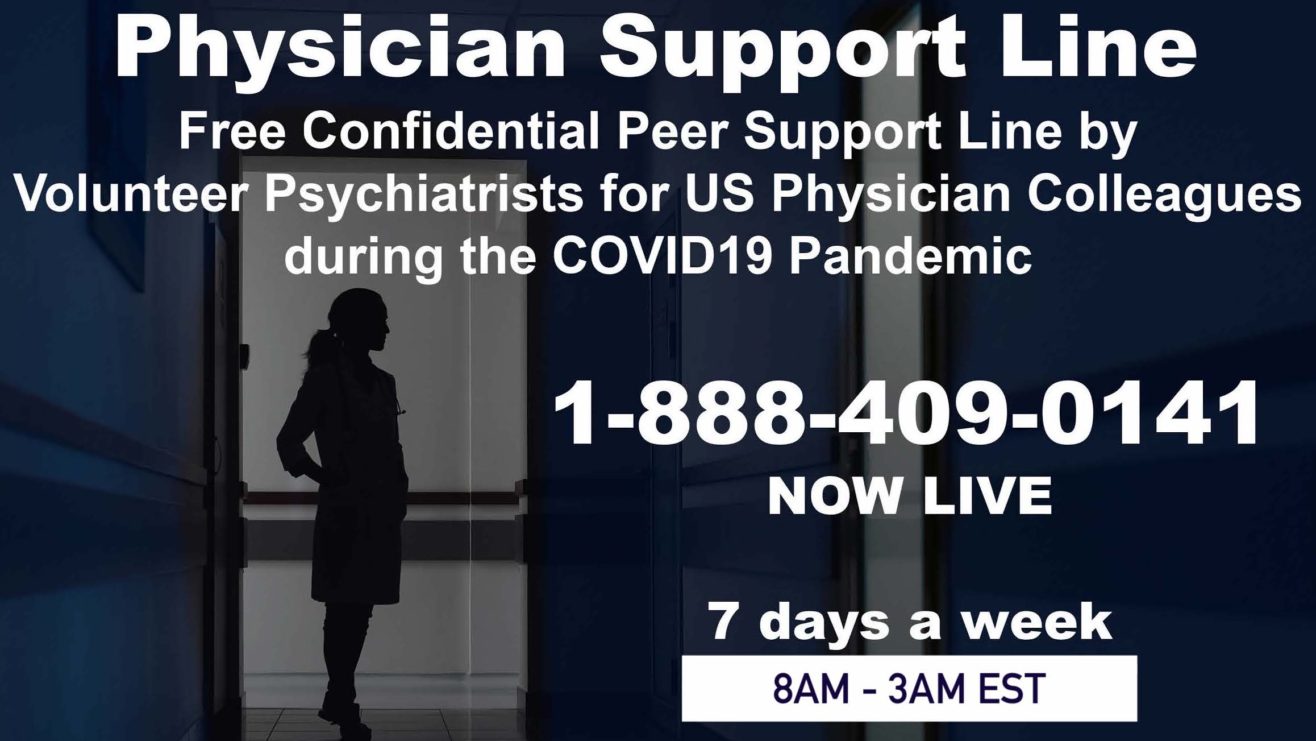
Physician Wellness Must be a Priority
Wellness Resources
Meditation & Body
Well-Being
Happiness & Unwinding
The Physicians Foundation’s 2023 Survey of America’s Current and Future Physicians
Key Findings
Summary of Survey

The state of physician wellbeing—for both current and future physicians—remains low.
- For the third year in a row, 6 in 10 physicians often have feelings of burnout, compared to 4 in 10 in 2018.
Physicians Reporting Feelings of Burnout
Residents Reporting Feelings of Burnout
Medical Students Reporting Feelings of Burnout
Medical students’ overall wellbeing is lower than both residents and physicians
- Three-quarters of medical students have felt inappropriate feelings of anger, tearfulness or anxiety, much more compared to residents (68%) and physicians (53%).
- More than half of medical students (55%) have felt hopeless or that they have no purpose, greater compared to residents (43%) and physicians (34%).
- Nearly two-thirds of medical students have felt levels of debilitating stress, much more compared to residents at 45%.
Current and future physicians need systems and workplaces to prioritize physician wellbeing and perspectives
- Only 31% of physicians agree that their workplace culture prioritizes physician wellbeing, declining from 36% a year ago.
- 50% of physicians or more shared that their workplace rarely or never takes action on 8 of the 16 evidence-based wellbeing solutions identified to support physicians.
- At least half of physicians and residents report third-part involvement, including insurance requirements, documentation protocols, regulatory policies and mandatory training requirements, consistently hinder their autonomy to deliver high-quality and cost-efficient care.
Current and future physicians report stigma and structural barriers affect their overall wellbeing and mental health.
- Nearly 8 in 10 physicians (78%), residents (79%) and medical students (76%) agree that there is stigma surrounding mental health and seeking mental health care among physicians.
- Approximately half of physicians (48%), residents (48%), and students (55%) said they know a physician/colleague/peer who said they would not seek mental health care.
- 4 in 10 physicians were either afraid or knew another physician fearful of seeking mental health care given questions asked in medical licensure/credentialing/insurance applications.